Ulcerative colitis is a chronic inflammatory bowel disease that causes inflammation in the inner linings of the colon and rectum. Ulcerative colitis is characterized by various gastrointestinal symptoms, including bloody diarrhea, abdominal pain, fatigue, and weight loss. The exact cause of ulcerative colitis remains unknown, however autoimmune conditions, bacterial or viral infections, and imbalances of the gut microbiota are believed to be significant in its development.
The management of ulcerative colitis in conventional medicine involves medications like non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and immunosuppressants. However, medication therapy can cause significant side effects and is generally unsuitable for long-term use, leaving many patients seeking a safer and more holistic alternative.
Functional medicine addresses the root causes of ulcerative colitis instead of just alleviating symptoms. The patient-centered approach of functional medicine emphasizes lifestyle and dietary changes, using the 5-Rs program. The 5-Rs program involves removing pro-inflammatory foods, replacing them with nutritious, anti-inflammatory options, reinoculating the gut with beneficial probiotics, repairing the gut lining, and rebalancing the gut and body.
This article will consider the symptoms, causes, and natural treatment of ulcerative colitis using functional medicine.
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory disease of the colon (the large intestine) and the rectum (the connection between the large intestine and the rectum). Ulcerative colitis is most common between 30 and 40 years of age., and is characterized by relapsing and remitting inflammation and ulcers on the inner lining of the colon and rectum,
Recurring and remitting inflammation means the occurrence of inflammation and ulcers “comes and goes.” The term “chronic” is generally used for any condition that lasts more than 1 year. However, in the context of ulcerative colitis, chronic means lifelong. So, once this condition develops, it lasts the rest of the individual’s life.
Ulcerative colitis is one of the inflammatory bowel diseases (IBDs), with the other being Crohn’s disease. IBDs affect more than 1 million people in the United States in total, with ulcerative colitis accounting for more than 60% of cases. Perhaps more concerning is the fact that ulcerative colitis is still on the rise in the country and around the world, with its incidence and prevalence ever-increasing.
What are the Symptoms of Ulcerative Colitis?
The symptoms of ulcerative colitis are mostly gastrointestinal, and they include bloody stool, mucus in stool, diarrhea, irregular bowel movements, and a false urge to empty the bowels. However, ulcerative colitis can also cause fatigue, fever, weight loss, and weakness.
Ulcerative colitis is a lifelong condition, and although its symptoms can be pretty severe at its peak, it generally starts on a milder note. Here are some of the symptoms associated with ulcerative colitis:
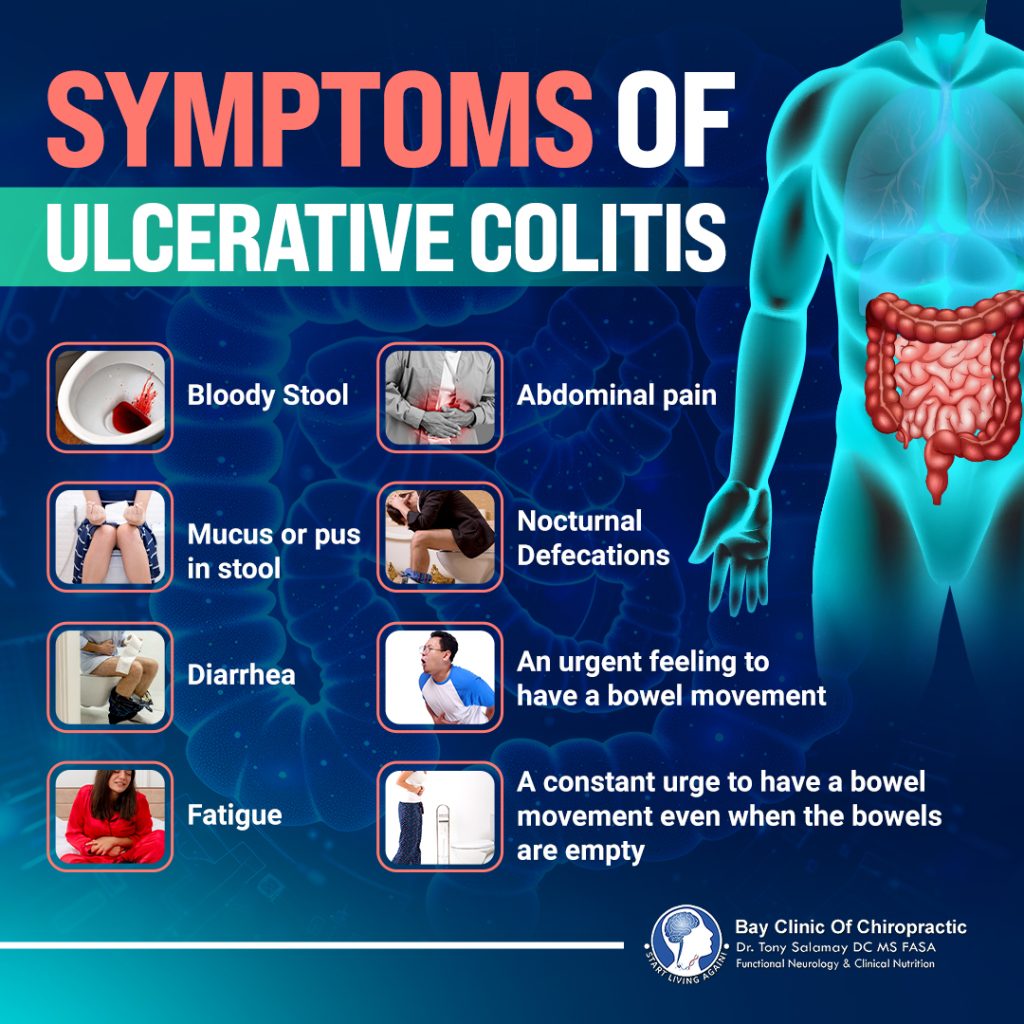
- Bloody stool
- Mucus or pus in stool
- Diarrhea
- Fatigue
- Abdominal pain
- Nocturnal defecations
- An urgent feeling to have a bowel movement
- A constant urge to have a bowel movement even when the bowels are empty
The symptoms of ulcerative colitis usually start mild. For instance, the individual may have bowel movements around 4 times a day at the start of the condition and may occasionally have blood in their stool. The person may have more than 6 bowel movements a day as the condition progresses, and most of these stools are bloody.
There may also be fever, weight loss, nausea, and body weakness. The other symptoms experienced in severe ulcerative colitis depend on how much of the colon is affected. Extremely severe cases may be characterized by more than 10 bloody stools in a day.
The general rule with ulcerative colitis is that mild symptoms progress to severe symptoms. However, a significant proportion of individuals (15%) can still have severe disease at the initial stage of the disease. Individuals with severe disease at the initial stage of the disease immediately have these gastrointestinal symptoms in addition to fever, fatigue, nausea, and weight loss.
What are the Causes of Ulcerative Colitis?
The exact cause of ulcerative colitis is unknown, although autoimmune conditions, bacterial or viral infections, and gut microbiota imbalances are widely accepted theories. Factors like genetics, ethnicity, and environmental factors like smoking can also contribute to the development of the condition.
There have been different theories over the years for what causes ulcerative colitis. The most common theory for the cause of ulcerative colitis is an autoimmune condition (a condition where the immune system mistakes the body’s cells as foreign and attacks them). The autoimmune attack will be on cells and tissues in the colon in the case of ulcerative colitis. Other common theories are the presence of certain bacterial or viral infections and an imbalance of the bacteria in the gut.
Despite there not being one single, widely accepted theory, it is generally agreed that there are complex risk factors associated with ulcerative colitis. They include:

- Genetics, with up to 11% of people with this condition having family members that also have it
- Ethnicity, with Jewish populations having higher rates of ulcerative colitis than any other ethnicity
- Gut microbiota
- Environmental and lifestyle factors, particularly smoking, increased stress, and poor diet
- Underlying health conditions, like gastroenteritis (stomach flu), appendicitis
- Medications, like oral contraceptives, non-steroidal anti-inflammatory drugs (NSAIDs – ibuprofen, diclofenac, aspirin), hormone replacement therapy.
Conventional Treatment of Ulcerative Colitis
Ulcerative colitis is managed primarily with medications in conventional medicine. The medications recommended are typically NSAIDs, corticosteroids, immunosuppressants, and biologics therapy for ulcerative colitis. What medication is used greatly depends on the severity and extent of the condition.
The next step may be surgery if there is still no improvement after using medications, and surgery typically involves the removal of the large intestine. The efficacy of medications in managing ulcerative colitis is very rarely an issue, but considering the chronic nature of the condition, the risk of safety problems greatly increases.
For example, NSAIDs can cause gastrointestinal bleeding, stomach ulcers, kidney issues, and liver problems. Steroids and immunosuppressants for ulcerative colitis can also greatly weaken the immune system, exposing the body to a wide range of infections. Also, the cost implication may be far too great for many, especially when you factor in the lifelong nature of these conditions.
Therefore, there is always ongoing research to find treatment options that can manage ulcerative colitis in both a safe and effective way. One of the most promising treatment options to emerge from this research is functional medicine.
Functional Medicine Treatment of Ulcerative Colitis
Functional medicine is a patient-centered form of alternative medicine that focuses on treating and managing medical conditions by addressing their root causes. This type of medicine considers the complex interactions between the body and its different parts, as well as the body and the environment. In simple words, it focuses on balancing the “whole system.” Another name then for functional medicine for ulcerative colitis is holistic medicine for ulcerative colitis.
Functional medicine can be effective in relieving the symptoms of ulcerative colitis, improving overall health along the way. Below, we will consider how functional medicine achieves this.
Diagnosis
The first step in the treatment of any condition in all forms of medicine is a diagnosis of the condition. Treatment success depends heavily on the accuracy of diagnosis. Functional medicine places a strong emphasis on proper diagnosis and testing.
The diagnosis process for ulcerative colitis usually follows the following pattern.
Patient History and Examination
A patient’s medical history includes information about the past medical conditions the patient has had, as well as previous surgeries, allergies, and vaccinations. Physical examination involves a health practitioner examining a patient and trying to manually gain information about their condition. The results of previous physical examinations may also be in the patient’s medical history record.
There is a relationship between genetics and ulcerative colitis, as studies from the World Journal of Gastroenterology have shown. Your risk of having ulcerative colitis increases if your family members have ulcerative colitis. Therefore, one of the first steps of diagnosis is your healthcare provider asking questions and examining your family history.
You can also expect questions about where you live, work, and the foods and drugs you take considering that ulcerative colitis is also linked to environmental factors, medication use, and underlying health conditions. Then, you may have to describe your symptoms, their severity, and when they first started. Aside from your history, your healthcare provider may physically examine you, especially your abdomen.
Testing
Testing is important in diagnosis as it tells biochemical information about the patient through a laboratory examination of their blood, saliva, urine, or other body samples. Physical examination and patient history can only tell so much. Healthcare providers rely on different tests for more accuracy in diagnosis. These tests include:
- Blood tests, which are used to check for anemia (a complication of ulcerative colitis), assess kidney health, and also check for signs of infections
- Stool tests, which are used to detect the presence of inflammation and other infections
- Endoscopic tests, which are usually done to see the inside of the colon and rectum
- Imaging tests, including X-ray, MRI (magnetic resonance imaging), and CT (computed tomography) scans, for finding tissue inflammation
Treatment
The primary goal of ulcerative colitis treatment is to induce and maintain remission in patients. Remission means an improvement in the symptoms of the patient and their quality of life. Typically, healthcare providers will have remission targets, including the cessation of bleeding in stools, a reduction of the frequency of stooling, and the healing of the colon and rectum.
The next step after hitting the primary goal of treatment is ensuring that the patient’s quality of life in the long term is good. An implication of this is that complications and disability are reduced to the barest minimum. Healthcare providers only consider ulcerative colitis well-managed after the short- and long-term goals of treatment are reached.
The foundation of the functional medicine approach to managing ulcerative colitis is nutritional therapy and lifestyle changes. Let’s break that down further.
Nutritional Therapy
Nutritional therapy is the use of diet to treat health conditions and maintain health. The role of diet in maintaining health is one of the building blocks of the functional medicine model for managing health conditions and maintaining health.
For example, in the management of inflammatory conditions, foods that contain inflammatory agents can make the condition much worse to manage. The same nutrition principle carries over to the management of ulcerative colitis.
The nutritional therapy used for the management of ulcerative colitis is known as the 5-Rs program. The Rs stand for remove, replace, re-inoculate, repair, and rebalance. Alternative medicine for ulcerative colitis first removes the foods that can be triggering ulcerative colitis flare-ups and destroying the lining of the colon and rectum. Some of the foods implicated in inflammatory processes include sweets, refined sugars, red and processed meat, sugary drinks, snacks, and other ultra-processed foods.
The next phase following the removal of these foods is their replacement with healthier, more beneficial foods for the colon and the rectum. The replacement phase usually involves adding foods and supplements that can reduce excess inflammation in the body. Examples of these foods are green leafy vegetables, fruits, whole grains, fatty fish, nuts, and legumes. Likewise, common examples of these anti-inflammatory supplements are turmeric, ginger, garlic, cinnamon, bromelain, green tea, quercetin, and vitamin D.

The next R stands for re-inoculate, and this R translates to reintroducing friendly bacteria into the gut. Friendly gut bacteria are probiotics which can help in the improvement of digestive symptoms.
Then, the repair phase comes up. In the repair phase, the use of supplements, vitamins, and other natural agents that can help repair the damaged lining of the large intestine is considered. The final stage, then, is the rebalance stage, which focuses on establishing a long-term nutritional plan that will keep the intestine in a state of continued balance. Rebalancing the intestine ensures that remission lasts long.
Lifestyle Changes
Making changes to some activities and routines of a patient’s lifestyle is often useful in managing health conditions. Although the 5-Rs program focuses mainly on nutrition, its concept also applies to lifestyle changes. Functional health practitioners will emphasize to someone trying to manage ulcerative colitis the need to remove habits and environmental factors that can trigger and worsen inflammation.
Functional health practitioners also advise the individual to add positive activities to their daily routine that can help heal the intestine and promote remission. Generally, activities to stop will include smoking, stress eating, and limiting exposure to environmental toxins and infections. Then, practicing mindfulness and stress-relieving exercises can help rebalance the mind and promote overall well-being.
Frequently Asked Questions
Is There a Cure for Ulcerative Colitis?
No, there is currently no cure for ulcerative colitis. However, colectomy (a surgical procedure that removes the entire colon) can effectively and permanently end all symptoms. We do not consider colectomy a cure, though. Despite there being no cure, there are treatment options, including functional medicine, that can help manage ulcerative colitis, providing relief from its symptoms and possibly reducing the frequency of flare-ups.
Do You Need Surgery for Ulcerative Colitis?
No, you generally will not need surgery for ulcerative colitis, except if the condition is at a severe stage or other treatment options have failed to produce any effective relief. The standard surgical procedure is a proctocolectomy, which removes the large intestine (including the colon and rectum).
Can Ulcerative Colitis Go Away on Its Own?
Most ulcerative colitis cases will not go away on their own if left untreated, instead worsening as the condition progresses into more advanced stages. Note that the symptoms of the condition going away for some time is not a sign that the condition has healed. The stage of temporary relief is called remission, and the symptoms may return after a few months or even years. Getting professional treatment is always your best bet in the management of ulcerative colitis.
Are Medications Safe for Treating Ulcerative Colitis?
The safety of medications for ulcerative colitis depends heavily on the duration of use. Medications have few safety risks when used for short-term relief of some ulcerative colitis symptoms. However, using medications for extended periods poses several safety risks due to the inherent side effects of the medications. Most people who rely solely on medications may have to use them for a very long time as ulcerative colitis is a chronic condition. Therefore, the risk of side effects and health problems is higher.
How is Ulcerative Colitis Diagnosed?
Ulcerative colitis is diagnosed through a comprehensive approach that includes collection of patient history, physical examination, and testing. Some of the key tests used include blood tests for anemia and infection, stool tests for inflammation, and imaging tests like X-rays and MRI scans for tissue inflammation.
Conclusion
Ulcerative colitis is a type of chronic inflammatory condition that affects hundreds of thousands of Americans. The treatment of ulcerative colitis in conventional medicine is generally limited to medications and surgery. However, considering the cost implication and safety concerns with some of these treatments, the functional medicine approach is on a steady rise.
Functional medicine is all-natural, personalized, and focuses on addressing the condition in a holistic manner. The specifics of the functional medicine approach is a nutritional therapy that comprises removing pro-inflammatory foods, replacing them with healthier foods and supplements, re-inoculating the intestine with probiotics, repairing the damaged intestine, and rebalancing the gut and body system.
Functional medicine advice and strategies cannot and should not replace direct recommendations from your healthcare provider, as each individual has different health needs, especially if you have underlying conditions or are on medication.
To get guidance and support from a dedicated and compassionate Functional Medicine Doctor in Panama City, Florida, contact the Bay Clinic of Chiropractic at (850) 785-9372 or info@thebaydoctor.com.
References
- Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. The Lancet [Internet]. 2016 Dec 1;389(10080):1756–70. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6487890/
- Digestive Diseases Statistics for the United States [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. 2025. Available from: https://www.niddk.nih.gov/health-information/health-statistics/digestive-diseases
- Kappelman MD, Moore KR, Allen JK, Cook SF. Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Digestive Diseases and Sciences [Internet]. 2012 Aug 28;58(2):519–25. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3576554/
- Symptoms & Causes of Ulcerative Colitis [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. 2025. Available from: https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/symptoms-causes
- Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal World Congress of Gastroenterology. Canadian Journal of Gastroenterology [Internet]. 2005 Jan 1;19(suppl a):5A-36A. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1155/2005/269076
- Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG Clinical guideline: Ulcerative colitis in adults. The American Journal of Gastroenterology [Internet]. 2019 Feb 27;114(3):384–413. Available from: https://journals.lww.com/ajg/fulltext/2019/03000/acg_clinical_guideline__ulcerative_colitis_in.10.aspx
- Dignass A, Eliakim R, Magro F, Maaser C, Chowers Y, Geboes K, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis Part 1: Definitions and diagnosis. Journal of Crohn S and Colitis [Internet]. 2012 Oct 3;6(10):965–90. Available from: https://academic.oup.com/ecco-jcc/article/6/10/965/503827?login=false
- Website N. Causes [Internet]. nhs.uk. 2022. Available from: https://www.nhs.uk/conditions/ulcerative-colitis/causes/
- Wen Z, Fiocchi C. Inflammatory bowel disease: autoimmune or immune-mediated pathogenesis? Journal of Immunology Research [Internet]. 2004 Jan 1;11(3–4):195–204. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2486322/
- Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nature Reviews Gastroenterology & Hepatology [Internet]. 2015 Mar 3;12(4):205–17. Available from: https://www.nature.com/articles/nrgastro.2015.34
- Halme L. Family and twin studies in inflammatory bowel disease. World Journal of Gastroenterology [Internet]. 2006 Jan 1;12(23):3668. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4087458/
- Karban A, Eliakim R. Effect of smoking on inflammatory bowel disease: Is it disease or organ specific. World Journal of Gastroenterology [Internet]. 2007 Jan 1;13(15):2150. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4146835/
- Di Re A, Liang Y, Gosselink MP, Ctercteko G. Acute Gastroenteritis in the Etiology of Inflammatory Bowel Disease: Systematic Review and Meta-analysis. Crohn S & Colitis 360 [Internet]. 2021 Sep 30;3(4). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9802281/
- The Risk of Oral Contraceptives in the Etiology of Inflammatory Bowel Disease: A Meta-Analysis [Internet]. ResearchGate. Available from: https://www.researchgate.net/publication/23153131_The_Risk_of_Oral_Contraceptives_in_the_Etiology_of_Inflammatory_Bowel_Disease_A_Meta-Analysis
- Ananthakrishnan AN, Higuchi LM, Huang ES, Khalili H, Richter JM, Fuchs CS, et al. Aspirin, nonsteroidal anti-inflammatory drug use, and risk for Crohn disease Ulcerative colitis: a cohort study. pmc.ncbi.nlm.nih.gov [Internet]. 2012 Mar 6; Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3369539/
- Khalili H, Higuchi LM, Ananthakrishnan AN, Manson JE, Feskanich D, Richter JM, et al. Hormone Therapy Increases Risk of Ulcerative Colitis but not Crohn’s Disease. Gastroenterology [Internet]. 2012 Jul 27;143(5):1199–206. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3480540/
- Treatment for ulcerative colitis [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases. 2025. Available from: https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/treatment
- Ghlichloo I, Gerriets V. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) [Internet]. StatPearls – NCBI Bookshelf. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547742/
- Ruiz R, Kirk AD. Long-Term toxicity of immunosuppressive therapy. In: Elsevier eBooks [Internet]. 2015. p. 1354–63. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7152453/
- Hanaway P. Form follows function: a functional medicine overview. The Permanente Journal [Internet]. 2016 Oct 14;20(4). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5101104/
- Strobel TM, Nguyen C, Riggs T, Horst SN, Motley A, Upadhyaya S, et al. Functional Medicine approach to patient care improves sleep, fatigue, and quality of life in patients with inflammatory bowel disease. Crohn S & Colitis 360 [Internet]. 2022 Jul 1;4(3). Available from: https://academic.oup.com/crohnscolitis360/article/4/3/otac032/6694181#381581605
- Ghavidel A. Ulcerative Colitis Associated with Aplastic Anemia; A Case Report [Internet]. 2013. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3990149/
- Moss AC. Residual inflammation and ulcerative colitis in remission [Internet]. 2014. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4014050/
- Scheller B, Winter C, Zamyad J, Felmlee K, Heard D. The successful management of ulcerative colitis with a nutritional intervention: a case report [Internet]. 2019. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7219448/
- Asensi MT, Napoletano A, Sofi F, Dinu M. Low-Grade Inflammation and Ultra-Processed Foods Consumption: A review. Nutrients [Internet]. 2023 Mar 22;15(6):1546. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10058108/
- Hungin APS, Mitchell CR, Whorwell P, Mulligan C, Cole O, Agréus L, et al. Systematic review: probiotics in the management of lower gastrointestinal symptoms – an updated evidence‐based international consensus. Alimentary Pharmacology & Therapeutics [Internet]. 2018 Feb 20;47(8):1054–70. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5900870/