Irritable Bowel Syndrome (IBS) is a prevalent gastrointestinal condition that affects up to 45 million people in the United States. While many gastrointestinal conditions do not last more than a few days, irritable bowel syndrome lasts a lifetime.
IBS is characterized by symptoms such as abdominal pain, constipation, diarrhea, and bloating. The exact causes of IBS remain unclear, although stress, imbalances in the gut microbiota, hormonal changes, and genetic factors may contribute to the development of the condition.
Despite the uncertainty about its causes, IBS is a manageable condition, with standard treatment options being conventional and functional medicine. Conventional medicine often focuses on symptomatic relief, using medications like antispasmodics and antidepressants without addressing underlying causes.
In contrast, the IBS functional medicine approach prioritizes personalized and holistic treatment for IBS that targets root issues. The functional medicine treatment plans include dietary changes, supplement use, and lifestyle recommendations like mindfulness, exercise, meditation, yoga, chiropractic, and physical therapy.
This article considers the symptoms, causes, and functional medicinal approach to managing irritable bowel syndrome.
What Is Irritable Bowel Syndrome?
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal condition characterized by abdominal pain and altered bowel habits. Depending on the exact change in bowel habits, IBS can be divided into three main categories: IBS-D (diarrhea-dominance), IBS-C (constipation-dominance), and IBS-M (dominance of both diarrhea and constipation). IBS is not a single condition but a group of intestinal symptoms that occur together.
Irritable bowel syndrome is also the most common functional gastrointestinal disorder. In total, IBS is responsible for close to $30 billion in medical costs in the United States and is also one of the biggest reasons people miss work every year. So, it is a bit surprising that the condition is so frequently overlooked in the medical world and by patients.
Well, one of the reasons for this overlooking is the fact that many people don’t even know they have the condition. And, it’s not just the patients. There are even health professionals who do not know about this condition, possibly because the condition has functional roots, which conventional medicine frequently overlooks. Regardless, the right information about how the condition presents can be helpful in quick diagnosis and treatment of the condition. Treatment starts with knowing some of its symptoms.
What are the Symptoms of Irritable Bowel Syndrome?
The symptoms of IBS include constipation, diarrhea, and general stomach discomfort. IBS symptoms are heavily influenced by the type of IBS in the first place. IBS-D (diarrhea-dominant IBS) will have more diarrhea symptoms than IBS-C (constipation-dominant IBS).
Regardless, some pretty common symptoms are experienced across the different categories of the condition. We will list all of these symptoms below.
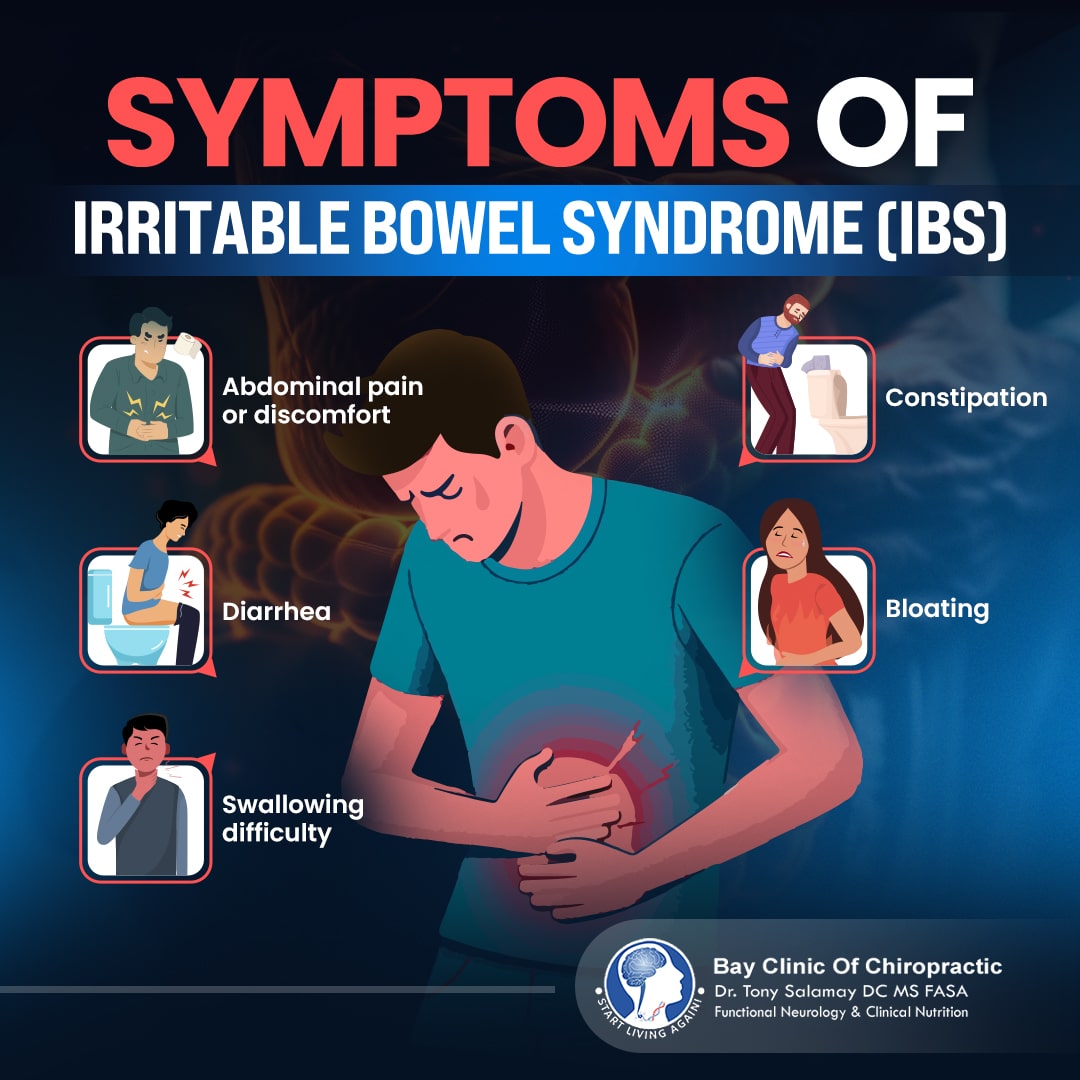
- Abdominal pain or discomfort
- Constipation
- Diarrhea
- Bloating
- Swallowing difficulty
While the condition is generally not life-threatening, the impact of these symptoms on the patient’s quality of life can be pretty significant. However, there may be instances where the condition is worrying and has pretty serious symptoms, including unexplained weight loss, rectal bleeding, anemia, colon cancer, celiac disease, and inflammatory bowel disease.
Sometimes, symptoms may also extend beyond the intestine. For example, there may be reduced sexual function, painful intercourse, hypertension, asthma, fibromyalgia (widespread pain and fatigue), and an increased frequency of urination.
What are the Causes of Irritable Bowel Syndrome?
Irritable bowel syndrome does not have any physically identifiable cause. However, one of the most common theories from research at the UCLA School of Medicine, Los Angeles, California, USA is that the condition is due to the impact of stress – both physical and psychological – on the body.
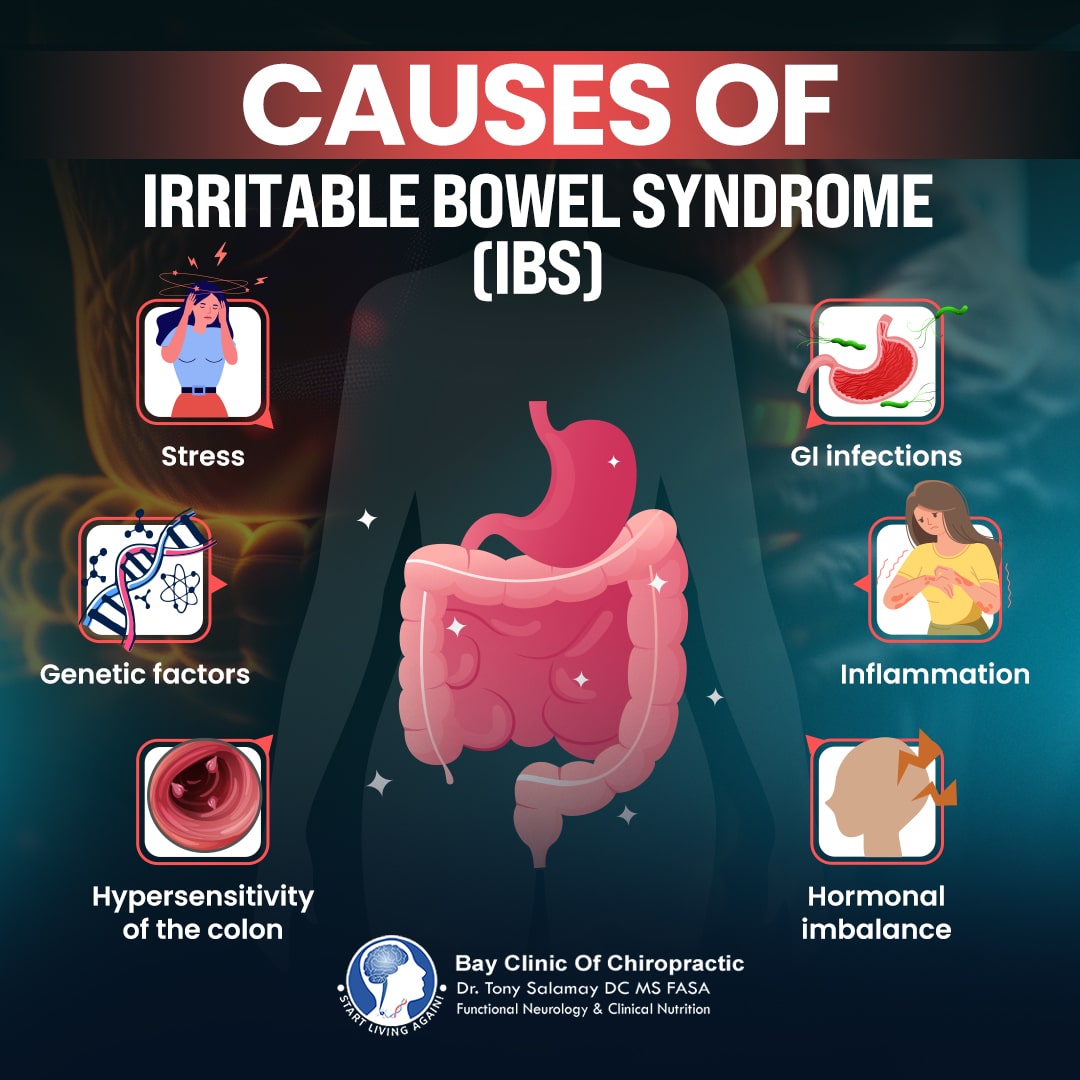
Another theory is that the colons (large intestines) of people with this condition are much more sensitive to factors like infection, chronic inflammation, gastrointestinal microbiota (microorganisms living in the gut), physical stimulation, stress, food, and certain hormones (cholecystokinin and corticotrophin-releasing hormone). Furthermore, an imbalance of the gut microbiota is thought to play a key role in irritable bowel syndrome. The gut microbiota can directly influence several gastrointestinal conditions and symptoms.
Other theories include an imbalance in the hormone serotonin, low-grade inflammation, gastrointestinal infections, and genetic factors. Irritable bowel syndrome also affects more women than men, which is an indicator that the biological and physical differences that exist between both sexes (and even different individuals of the same sex) can play a part in the development of the condition.
Conventional Treatment of Irritable Bowel Syndrome
One of the trends frequently observed in conventional medicine is that the management of different conditions is often restricted to the management of its symptoms. This trend is even more so when you have conditions without a clearly defined cause, like IBS. Therefore, the conventional management of IBS is largely symptomatic.
The irritable bowel syndrome medication treatment addresses the individual symptoms the patient presents with. Classic cases include the use of antispasmodics and antidepressants for abdominal pain, laxatives for constipation, and loperamide (an anti-diarrheal agent) in managing diarrhea. Some other medications conventional health practitioners recommend are tegaserod, antibiotics, and alosetron.
Having a treatment option that can provide immediate relief is always an advantage, no doubt, but the long-term use of such a medication starts to bring different problems. The use of any drug for extended periods increases the chances of having adverse drug effects, which all drugs can potentially cause. Considering that irritable bowel syndrome is a lifetime condition, you can see our point, especially with medications like antidepressants and antibiotics, which can have significant side effects. Interestingly, the efficacy of some of these drugs is unproven, casting further doubts about even their short-term use.
Also, medications simply mask the symptoms of the condition, meaning the root causes and triggers of the condition remain even when the symptoms are managed. Put another way, the patient will only feel temporary relief; the symptoms will very likely just spring up again, and may even get progressively worse. The ideal management of IBS will be a treatment that can not only relieve symptoms, but also address the possible root causes of the condition and help in actually managing it.
Functional Medicine Treatment of Irritable Bowel Syndrome
Functional medicine is an evidence-based, patient-centered, root-cause-focused type of medicine that aims to achieve holistic medicine treatment of health conditions. Simply, functional medicine is backed by science, centered around patients and their individual differences, and also guided by the possible root causes of the condition. Therefore, the eventual care gotten is personalized and treats the whole body system, improving the overall quality of life.
Close to half of people with IBS turn to IBS alternative medicine, which is unsurprising since the safety and efficacy of functional medicine are backed by both patient-reported and clinical evidence. Treatment usually starts with reaching a diagnosis of the condition. The importance of this step cannot be overstated as there is no specific test that can diagnose IBS, so health practitioners often use tests to rule out other conditions and then combine the findings of the test with other patient information and symptoms.
Functional health experts may order stool tests to assess the state of the intestine and try to get an idea of the state of the gut microbiota. Blood tests can also help determine the presence of inflammation, another way IBS presents. The functional medicine doctor for IBS moves on to the actual treatment of the condition after reaching a diagnosis.
The goal of IBS treatment is to provide both short—and long-term relief to patients. Here are some of the standard irritable bowel syndrome treatment options.
Diet
Diet (foods and drinks) significantly influences the gut and the microorganisms living in it. There are foods that can positively promote the health of these microorganisms and help heal and grow the intestine. Likewise, there are foods that can contribute to the imbalance of the gut microbiota and worsen the state of the intestine. The simple plan in the management of IBS is to eliminate the “bad” foods and include the “good” ones.
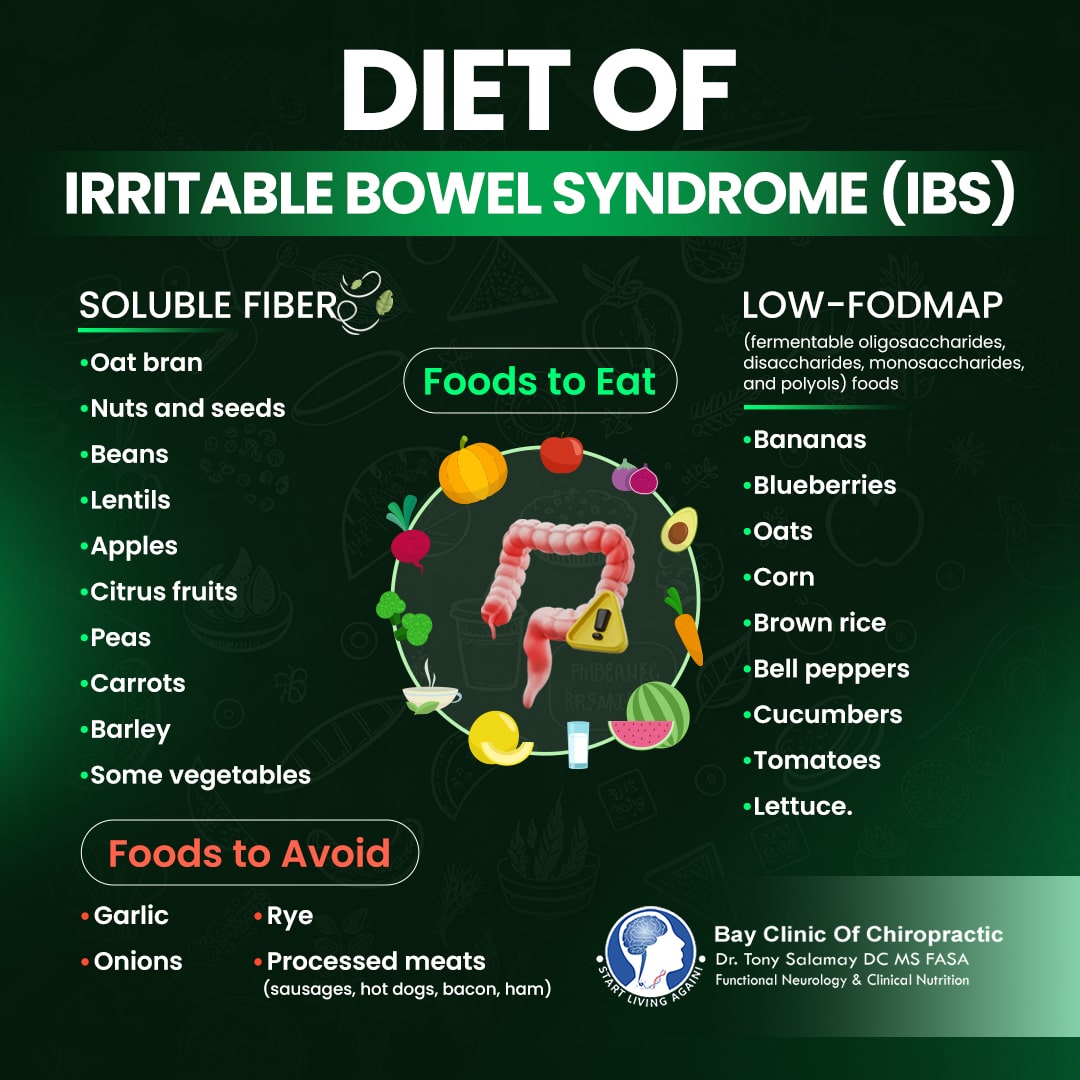
The removal of certain foods is known as an elimination diet, which has been proven to have good results in the management of IBS. Some of the more common foods that are eliminated include gluten, dairy, beef, pork, and caffeine. The trick is the removal of foods that can cause inflammation and also negatively affect the intestine and gut microbiota.
Functional health practitioners don’t just stop at removing certain foods; they have to add some other foods that can benefit the patient. One of the most commonly recommended classes of foods for IBS is soluble fiber, which is present in oat bran, nuts and seeds, beans, lentils, apples, citrus fruits, peas, carrots, barley, and some vegetables. These foods can help improve constipation and other general IBS symptoms.
Other foods that can help in the management of IBS are foods low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols). They include bananas, blueberries, oats, corn, brown rice, bell peppers, cucumbers, tomatoes, and lettuce. Conversely, garlic, onions, rye, and processed meats are foods high in FODMAPs.
Supplements
Supplements are products intended to support your overall diet and provide the nutrients that diet cannot adequately supply. Supplement use is a type of nutritional therapy in the management of IBS. Different supplements have been identified as beneficial to the gut and symptoms of IBS. Perhaps the most important group of such supplements is probiotics.
Defined as live organisms that exert health benefits when taken in adequate amounts, probiotics can help improve the symptoms of IBS, like pain, colonic sensitivity, and intestinal motility. You can take probiotic supplements, and there are also probiotic foods (yogurt, kefir, sauerkraut, miso, kombucha) that can help in the management of IBS. Another supplement that studies have found useful in the management of IBS symptoms is peppermint oil. Fiber supplements can also be helpful.

Supplements cannot and should not replace a healthy diet, regardless of health state and supplement type. Plus, you should talk to your healthcare provider before starting on any supplement if you have other underlying health conditions, especially of the gut.
Lifestyle Recommendations
Lifestyle recommendations are proposed alterations to normal lifestyle practices when managing health conditions or trying to improve overall health. Stress reduction is one of the main lifestyle interventions functional health practitioners recommend in the management of IBS. This recommendation comes in light of the role of stress in the development and progression of irritable bowel syndrome.
Examples of stress-reduction practices are mindfulness, exercise, breathing exercises, meditation, yoga, and tai chi. There’s no rule book here, though. Do whatever makes you feel relaxed, as long as it’s healthy.
Functional health practitioners may also recommend other therapies that can influence the balance of the gut and overall system, like chiropractic. Physical treatments, like massage, can also help improve the quality of life of patients.
Frequently Asked Questions
Is Irritable Bowel Syndrome Preventable?
There is no one single therapy or treatment option that can prevent irritable bowel syndrome. However, with the right treatment, including functional medicine, it is possible to reduce the risk of the condition developing, as well as its severity if it does develop. This is usually through different lifestyle and dietary changes.
Can Irritable Bowel Syndrome Be Cured?
There is no cure for irritable bowel syndrome, but it is very much possible to manage the symptoms of the condition and improve quality of life with the right treatment strategies. These strategies include eating certain foods and cutting some from an individual’s regular diet, supplementation, mind-body therapies, and lifestyle changes. Functional health practitioners can advise on these strategies.
Does Irritable Bowel Syndrome Go Away on Its Own?
Irritable bowel syndrome does not go away on its own or at all, for that matter. If you have IBS, you can expect to have it for the rest of your life, and the impact of its different symptoms on the quality of life can be quite significant. However, there are treatment options, including functional medicine, that can help relieve these symptoms and ensure a good quality of life. Therefore, if you have the condition or notice symptoms of the condition, do not hesitate to contact your healthcare provider and a functional health practitioner.
How Does Functional Medicine Treat Irritable Bowel Syndrome?
Functional medicine treats IBS by first identifying root causes of the condition and then drafting a personalized treatment plan, consisting of nutritional changes, supplement use, and lifestyle modifications. This holistic approach aims to relieve symptoms while promoting overall gut health, reducing inflammation, and improving the patient’s quality of life.
What Dietary Changes Can Help Manage IBS?
Dietary changes to manage IBS often revolve around adopting an elimination diet, which means removing certain foods from diet. Typical foods that functional health practitioners recommend to be cut from diet include pro-inflammatory foods, such as gluten and dairy. Also, incorporating soluble fiber-rich foods and low-FODMAP options, like bananas and oats, can contribute to symptomatic relief.
What Lifestyle Changes Can Improve IBS Symptoms?
Lifestyle changes that can improve IBS symptoms include stress reduction techniques like mindfulness, yoga, and meditation, regular physical activity, and therapies like chiropractic and massage. These lifestyle changes can enhance gut function, which help in relieving IBS symptoms and improving quality of life.
Conclusion
Irritable Bowel Syndrome is a chronic condition of the intestine, and its impact on quality of life can be very significant. While conventional treatments focus on managing symptoms, functional medicine offers a more holistic approach by addressing potential root causes and healing the general system. Through personalized dietary changes, supplements, and lifestyle interventions, patients can find both short-term and long-term relief.
Contacting functional health practitioners can be a game-changer in managing your condition if you’re experiencing symptoms. Remember, though, to not make drastic health changes, especially if you have underlying health conditions, without first talking to your healthcare provider.
References
- Häuser W, Layer P, Henningsen P, Kruis W. Functional bowel disorders in adults. Deutsches Ärzteblatt International [Internet]. 2012 Feb 3; Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3285279/
- Soares RL. Irritable bowel syndrome: A clinical review. World Journal of Gastroenterology [Internet]. 2014 Jan 1;20(34):12144. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4161800/
- Vahedi H, Ansari R, Mir-Nasseri M, Jafari E. Irritable bowel Syndrome: a review article [Internet]. 2010. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4154827/
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology [Internet]. 2006 Apr 1;130(5):1480–91. Available from: https://www.gastrojournal.org/article/S0016-5085(06)00512-9/fulltext?referrer=https%3A%2F%2Fpubmed.ncbi.nlm.nih.gov%2F
- Nathani RR, Sodhani S, Vadakekut ES. Irritable bowel syndrome [Internet]. StatPearls – NCBI Bookshelf. 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534810/
- Siracusa R, Di Paola R, Cuzzocrea S, Impellizzeri D. Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. International Journal of Molecular Sciences [Internet]. 2021 Apr 9;22(8):3891. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8068842/
- Mayer EA, Naliboff BD, Chang L, Coutinho SV. V. Stress and irritable bowel syndrome. AJP Gastrointestinal and Liver Physiology [Internet]. 2001 Apr 1;280(4):G519–24. Available from: https://journals.physiology.org/doi/full/10.1152/ajpgi.2001.280.4.G519?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
- Naliboff BD, Munakata J, Fullerton S, Gracely RH, Kodner A, Harraf F, et al. Evidence for two distinct perceptual alterations in irritable bowel syndrome. Gut [Internet]. 1997 Oct 1;41(4):505–12. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1891510/
- Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut [Internet]. 2002 Jul 1;51(Supplement 1):i41–4. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1867730/
- Wang C, Fang X. Inflammation and overlap of irritable bowel syndrome and functional dyspepsia. Journal of Neurogastroenterology and Motility [Internet]. 2021 Apr 2;27(2):153–64. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8026374/
- Pace F. Family history of irritable bowel syndrome is the major determinant of persistent abdominal complaints in young adults with a history of pediatric recurrent abdominal pain. World Journal of Gastroenterology [Internet]. 2006 Jan 1;12(24):3874. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4087936/
- Lee SY, Kim JH, Sung IK, Park HS, Jin CJ, Choe WH, et al. Irritable bowel syndrome is more common in women regardless of the menstrual phase: a Rome II-based survey. Journal of Korean Medical Science [Internet]. 2007 Jan 1;22(5):851. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2693852/
- Mayer EA. Irritable bowel syndrome. New England Journal of Medicine [Internet]. 2008 Apr 16;358(16):1692–9. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3816529/
- Ferguson JM. SSRI antidepressant medications. The Primary Care Companion for CNS Disorders [Internet]. 2001 Feb 1;3(1). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC181155/
- Papale AJ, Flattau R, Vithlani N, Mahajan D, Nadella S. A review of Pharmacologic and Non-Pharmacologic therapies in the Management of Irritable Bowel Syndrome: Current recommendations and evidence. Journal of Clinical Medicine [Internet]. 2024 Nov 18;13(22):6948. Available from: https://www.mdpi.com/2077-0383/13/22/6948
- Gordon JS. Holistic Medicine: Advances and shortcomings [Internet]. 1982. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1273970/
- Hanaway P. Form follows function: a functional medicine overview. The Permanente Journal [Internet]. 2016 Oct 14;20(4). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5101104/
- Shen YHA, Nahas R. Complementary and alternative medicine for treatment of irritable bowel syndrome [Internet]. 2009. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2642499/
- Spiegel BMR, Farid M, Esrailian E, Talley J, Chang L. Is irritable bowel syndrome a diagnosis of exclusion? A survey of primary care providers, gastroenterologists, and IBS experts. The American Journal of Gastroenterology [Internet]. 2010 Mar 2;105(4):848–58. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2887205/
- Wagner LE, Bridges KM, Hinman JM, He J, Buckles D, Dunn W, et al. Treatment of functional bowel disorders in an integrative medicine clinic resulting in improved digestive tract symptoms. JGH Open [Internet]. 2024 Jan 1;8(1). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10805498/
- Bijkerk CJ, Muris JWM, Knottnerus JA, Hoes AW, de Wit NJ. Systematic review: the role of different types of fibre in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2004;19:245-51. Available from: https://www.rima.org/web/medline_pdf/alimpharmther_245.pdf
- Böhn L, Störsrud S, Liljebo T, Collin L, Lindfors P, Törnblom H, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology [Internet]. 2015 Aug 5;149(6):1399-1407.e2. Available from: https://www.gastrojournal.org/article/S0016-5085(15)01086-0/fulltext?referrer=https%3A%2F%2Fpubmed.ncbi.nlm.nih.gov%2F
- Latif A, Shehzad A, Niazi S, Zahid A, Ashraf W, Iqbal MW, et al. Probiotics: mechanism of action, health benefits and their application in food industries. Frontiers in Microbiology [Internet]. 2023 Aug 17;14. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10470842/
- Sharma S, Kumar S, Sajjad S, Sharma S. Probiotics in Irritable bowel Syndrome: a review article. Cureus [Internet]. 2023 Mar 23; Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10122169/
- Alammar N, Wang L, Saberi B, Nanavati J, Holtmann G, Shinohara RT, et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC Complementary and Alternative Medicine [Internet]. 2019 Jan 17;19(1). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6337770/
- Vasant DH, Paine PA, Black CJ, Houghton LA, Everitt HA, Corsetti M, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut [Internet]. 2021 Apr 26;70(7):1214–40. Available from: https://gut.bmj.com/content/70/7/1214.long