Chronic pain makes even the simplest parts of your life feel unbearable. Getting out of bed, focusing at work, or enjoying time with loved ones becomes a challenge. The constant discomfort drains your energy and leaves you feeling frustrated and stuck.
Chronic pain is characterized by long-standing pain that occurs when your body’s pain signals remain active for over 3 months. Unresolved injuries, inflammation, or nerve damage often cause this persistent pain.
The symptoms can vary but often include:
- Ongoing pain that aches, throbs, or shoots
- Fatigue that never seems to fade
- Stiffness or limited mobility in your joints or muscles
- Disrupted sleep, leaving you exhausted and irritable
- Emotional toll, including anxiety and depression
In a study on the prevalence of chronic pain in United States adults, Dr. Catherine B. Johannes from RTI Health Solutions, Waltham, Massachusetts, USA, states “The overall crude point prevalence of self-reported chronic pain (pain lasting at least 6 months) was 34.5%”
Fortunately, understanding chronic pain opens the door to effective natural solutions. In this article, you’ll learn about natural treatments, including functional medicine, dietary changes, and herbal remedies, targeting chronic pain’s root causes. You’ll also discover the benefits of hot and cold therapy, yoga, and mindfulness for long-term relief.
Take charge of your chronic pain and explore how personalized care and proven strategies can transform your life. Keep reading and you’ll find the answers you’ve been searching for.
What Is Chronic Pain?
Chronic pain is pain lasting longer than 12 weeks, persisting beyond the usual healing time for an injury or illness. Unlike acute pain, which signals immediate harm to the body and subsides as healing occurs, chronic pain continues without a clear cause or despite treatment.
This ongoing pain can range from mild to severe and may come and go or remain constant. Chronic pain often affects daily life, making working, sleeping, or enjoying hobbies hard. It’s also linked to emotional and mental health challenges, like anxiety and depression.
Unlike acute pain, which serves a protective role, chronic pain doesn’t offer any benefits. It can result from nervous system changes or damage, making the pain more complex to treat. Understanding chronic pain’s characteristics helps determine appropriate treatments and improves quality of life.
Types of Chronic Pain
Chronic pain is a broad category encompassing various types, each with its own characteristics and underlying causes. Below are some of the most common types of chronic pain:
- Neuropathic Pain: Results from nerve damage or dysfunction. Common in conditions like diabetic neuropathy and sciatica, this pain often feels like burning, stabbing, or electric shocks. In a study on neuropathic pain, Dr. Luana Colloca from the University of Maryland, USA, states “Neuropathic pain can substantially impair quality of life”
- Nociceptive Pain: Caused by tissue damage or inflammation, such as in arthritis or muscle injuries. It often presents as aching or throbbing.
- Central Pain Syndrome: Affects the central nervous system, causing widespread pain and sensitivity, as seen in fibromyalgia or post-stroke pain.
- Musculoskeletal Pain: Affects the muscles, bones, ligaments, tendons, and joints, often described as aching, stiffness, or soreness. Common areas include back pain, neck pain, and shoulder pain.
- Chronic Post-Surgical or Post-Trauma Pain: Pain that lingers after healing from surgery or injuries, such as car accidents or fractures.
- Psychogenic Pain: Related to psychological factors like stress, depression, or past trauma, with no clear physical cause.
- Visceral Pain: Arises from the internal organs, often linked to conditions like irritable bowel syndrome (IBS) or endometriosis.
- Migraines and Headaches: They can range from mild to severe and often interfere with daily activities. Migraines are frequently accompanied by throbbing pain, nausea, vomiting, and sensitivity to light and sound
Mixed Types of Pain
Mixed pain involves a combination of nociceptive (tissue-related) and neuropathic (nerve-related) pain, making it more challenging to diagnose and treat. This type of pain arises when both tissue damage and nerve dysfunction contribute to symptoms, resulting in overlapping sensations. Patients may experience sharp, burning, or shooting pain (neuropathic) along with aching or throbbing discomfort (nociceptive).
Conditions like chronic back pain often fall into this category. For example, a herniated disc may compress nerves, causing neuropathic pain, while inflammation or muscle strain around the disc causes nociceptive pain. Cancer pain is another example, as tumors may damage both tissues and nearby nerves. Similarly, fibromyalgia combines central nervous system dysfunction with widespread muscle pain, creating a mix of pain types.
Treating mixed pain requires addressing both components simultaneously. Tailoring treatments to both aspects of the pain improves outcomes and quality of life for those affected by mixed pain syndromes.
What Are The Symptoms Of Chronic Pain?
The symptoms of chronic pain often manifest in both physical and emotional ways, affecting daily life and overall well-being.
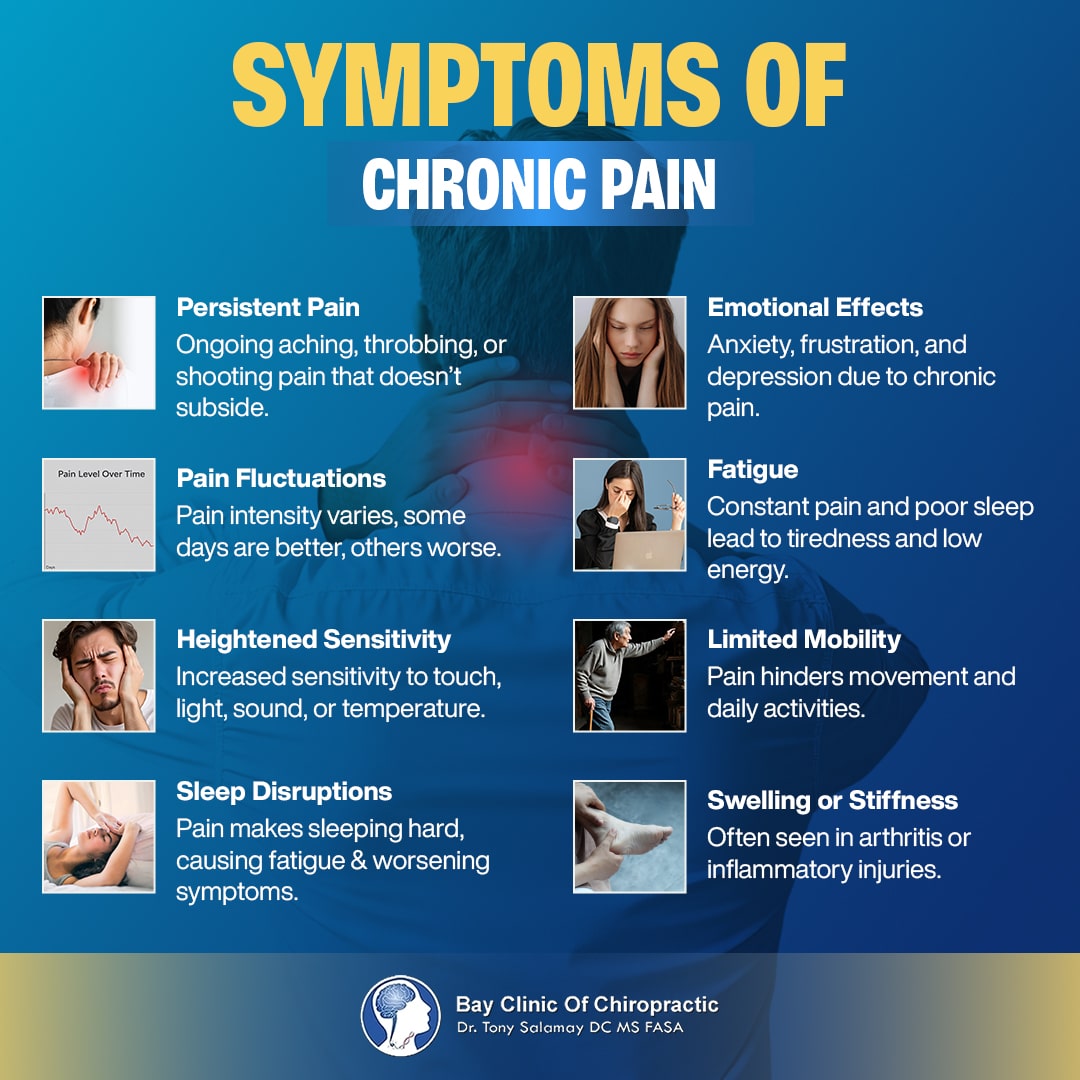
Here are the symptoms of chronic pain:
- Persistent Pain: Continuous or recurring pain described as aching, throbbing, or shooting that doesn’t go away.
- Pain Fluctuations: Pain levels may vary daily. Some days feel manageable, while others are worse.
- Heightened Sensitivity: Increased sensitivity to touch, light, sound, or temperature (hyperesthesia or allodynia).
- Sleep Disruptions: Difficulty falling or staying asleep due to pain, leading to exhaustion and worsening symptoms.
- Emotional Effects: Chronic pain often leads to anxiety, frustration, and depression because of its relentless nature.
- Fatigue: Persistent discomfort and poor sleep result in chronic tiredness and low energy.
- Limited Mobility: Pain can make moving or performing everyday activities hard.
- Swelling or Stiffness: Common in conditions like arthritis or injuries that involve inflammation.
What Causes Chronic Pain?
The causes of chronic pain are diverse, ranging from physical injuries to long-term medical conditions and psychological factors. Below are the most common causes of chronic pain.
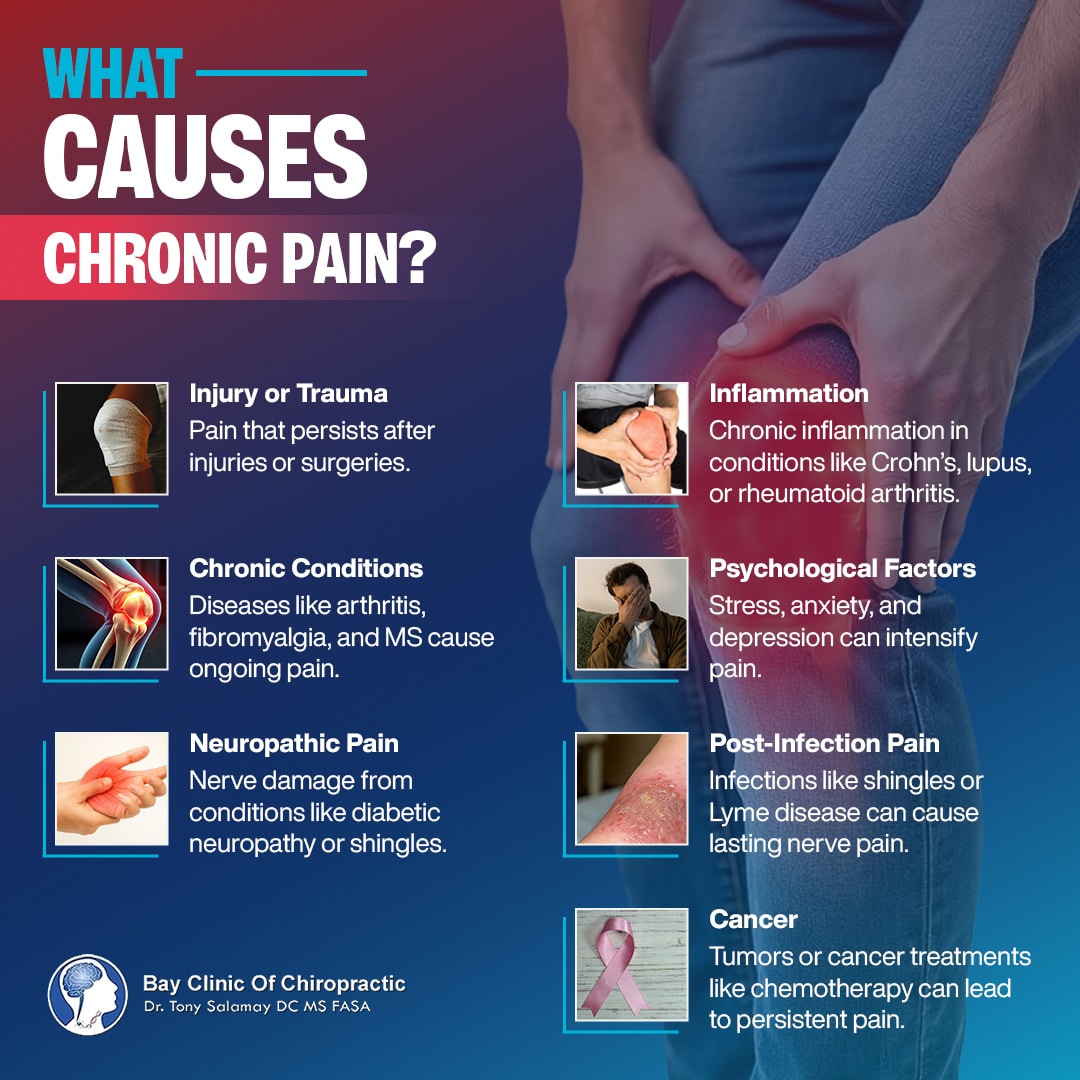
- Injury or Trauma: Pain that continues after healing from fractures, surgeries, or car accidents. In a study on chronic widespread pain after car accident injuries, Dr. Hu JunMei from the University of North Carolina, Chapel Hill, NC, USA, states “Motor vehicle collision (MVC) can trigger chronic widespread pain (CWP) development in vulnerable individuals.”
- Chronic Conditions: Diseases like arthritis, fibromyalgia, and multiple sclerosis are leading causes of persistent pain. Arthritis causes inflammation and gradual deterioration of the joints, leading to stiffness and discomfort, Fibromyalgia amplifies pain signals in the brain, causing widespread pain and fatigue. In multiple sclerosis, nerve damage interferes with pain processing, leading to chronic discomfort.
- Neuropathic Pain: Nerve damage or dysfunction, such as diabetic neuropathy, shingles, or spinal cord injuries. Damaged nerves send faulty signals to the brain, often resulting in sensations like burning, shooting, or electric-shock-like pain that can persist months or even years after the initial injury.
- Inflammation: Prolonged inflammation in conditions like Crohn’s disease, lupus, or rheumatoid arthritis often triggers ongoing pain. Chronic inflammation damages surrounding tissues over time, leading to stiffness, swelling, and restricted movement in affected areas.
- Psychological Factors: Stress, anxiety, and depression can worsen pain perception and create a vicious cycle of discomfort. Psychological factors amplify how your body processes pain signals, making sensations feel more intense than they would normally.
- Post-Infection Pain: Certain infections, like shingles or Lyme disease, can lead to chronic nerve pain even after the infection resolves. For example, post-infection neuralgia from shingles results from nerve damage caused by the viral infection, leaving pain that can last for months or years.
- Cancer: Tumors pressing on nerves or cancer treatments like chemotherapy can cause lasting pain. The growth of tumors may compress surrounding tissues and nerves, while chemotherapy can damage nerve endings, resulting in peripheral neuropathy.
Natural Treatments For Chronic Pain
Natural remedies offer a holistic approach to managing chronic pain by addressing the root causes and promoting overall well-being. These treatments focus on restoring balance to the body and mind, reducing inflammation, and supporting long-term healing. Unlike medications that often mask symptoms, natural approaches aim to address the underlying issues contributing to pain.
Functional Medicine
Functional medicine is a personalized approach that targets the root causes of chronic pain rather than just managing symptoms. Treating the body as an interconnected system helps restore balance and reduce pain naturally.
Chronic pain often arises from issues like poor nutrition, inflammation, or harmful environmental toxins. Functional medicine focuses on providing tailored nutrition plans to reduce inflammation and improve digestion, ensuring your body gets the nutrients it needs to heal. It also supports your body’s natural elimination processes by helping your liver and kidneys eliminate toxins like heavy metals, environmental toxins, or endotoxins from bacteria, which can worsen pain.
Imbalances in the immune system and hormones are also common contributors to chronic pain. Functional medicine works to calm chronic inflammation caused by immune system overactivity and correct hormonal imbalances, such as those involving the thyroid or adrenal glands.
By addressing these underlying factors, functional medicine alleviates pain and promotes long-term health and well-being.
Dietary Adjustments
What you eat plays a major role in managing chronic pain. Some foods can reduce inflammation and support healing, while others may trigger or worsen pain.
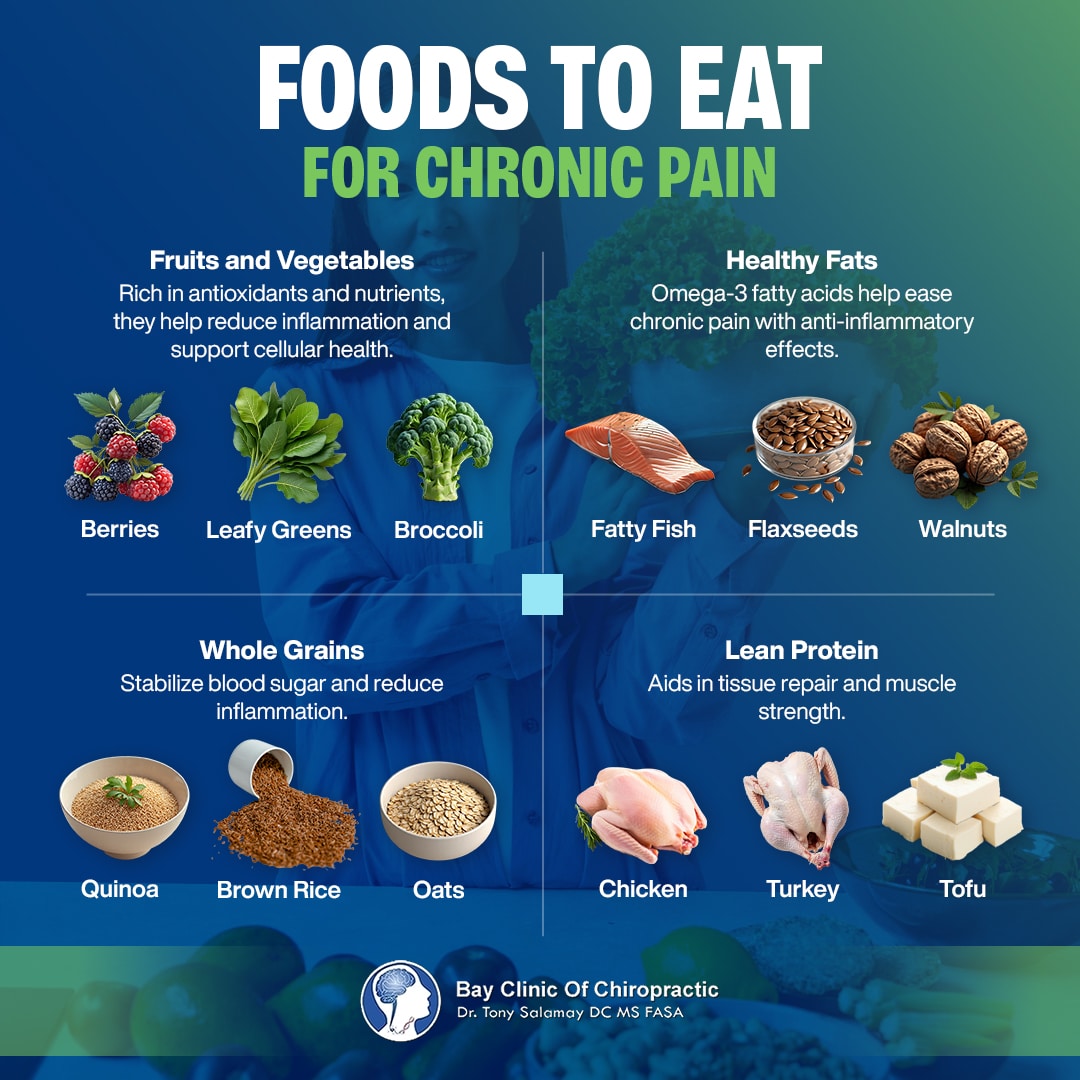
Here’s what to eat and what to avoid for chronic pain:
Foods to Eat for Chronic Pain
- Fruits and Vegetables: Packed with antioxidants and nutrients, fruits like berries and vegetables like leafy greens and broccoli help reduce inflammation and support overall cellular health.
- Healthy Fats: Omega-3 fatty acids in fatty fish like salmon, flaxseeds, and walnuts have strong anti-inflammatory properties that can ease chronic pain.
- Whole Grains (if tolerated): Nutrient-rich options like quinoa, brown rice, and oats stabilize blood sugar levels and help reduce inflammation.
- Lean Protein: Protein sources such as chicken, turkey, legumes, and tofu aid in tissue repair and maintaining muscle strength.
Foods to Avoid for Chronic Pain
- Processed Foods: Packaged snacks, fast food, and sugary treats increase inflammation due to additives and high sugar content.
- Refined Carbohydrates: White bread, pasta, and pastries spike blood sugar and can trigger inflammatory responses.
- Fried Foods: These foods are high in trans fats which worsen inflammation and contribute to weight gain.
- Alcohol: Excessive alcohol can disrupt immune function and exacerbate inflammation.
- Dairy: For some, dairy products can cause inflammation, especially if lactose-intolerant or sensitive.

Balancing your meals with protein, healthy fats, and complex carbohydrates helps stabilize blood sugar levels and supports overall energy. For instance, pair a lean protein like chicken or fish with a side of roasted vegetables and quinoa to provide sustained energy and minimize inflammation. Planning meals ahead also helps avoid the temptation of processed and inflammatory foods, keeping you on track to better manage chronic pain.
Chiropractic Care
Chiropractic care is a hands-on approach to treating chronic pain that focuses on aligning the spine and musculoskeletal system. Misalignments in the spine, called subluxations, can interfere with nerve function, leading to pain, reduced mobility, and other health issues. Chiropractors use gentle adjustments to correct these misalignments, promoting proper nerve communication and relieving pain at its source.
One of the key benefits of chiropractic care is its ability to address the root causes of chronic pain without relying on medication or invasive procedures. By improving spinal alignment, chiropractic adjustments may relieve nerve pressure, reduce inflammation, and restore mobility. This is particularly effective for conditions like back pain, neck pain, headaches, and joint pain.
Chiropractic care also helps improve posture and body mechanics, which can prevent further pain or injuries. Many patients report additional benefits, such as improved sleep, reduced stress, and greater well-being.
Regular chiropractic care can help maintain these improvements over time, offering a drug-free solution for managing chronic pain and enhancing overall health
Herbal Remedies
Herbal remedies have been used for centuries to manage chronic pain naturally. These plant-based treatments offer anti-inflammatory and pain-relieving properties without the potential side effects of long-term medication use. Consult a healthcare provider to determine the correct doses for your specific needs.
Here are our recommendations for herbal remedies for chronic pain:
Willow Bark
Willow bark, derived from willow trees’ bark, is a natural alternative to aspirin. Its active compound, salicin, converts to salicylic acid in the body, which reduces inflammation and alleviates pain. It has been traditionally used to treat arthritis, lower back pain, and headaches.
Willow bark works by blocking the production of prostaglandins, chemicals that contribute to inflammation and pain. Its effects are slower but longer-lasting than synthetic pain relievers, making it a preferred choice for chronic conditions.
Willow bark is available in several forms, including capsules, tinctures, and teas. Tea is made by steeping the dried bark in hot water. The typical daily dose of salicin is 120-240 mg. However, avoiding overuse is important, as excessive consumption may irritate the stomach lining.
Consult a functional medicine provider if you’re taking blood thinners or have allergies to aspirin before using willow bark.
Ginger
Ginger is a well-known natural remedy with potent anti-inflammatory and antioxidant properties. It contains active compounds called gingerols and shogaols that inhibit the production of inflammatory chemicals in the body, such as prostaglandins and leukotrienes.
Ginger is particularly effective in reducing pain caused by osteoarthritis, rheumatoid arthritis, and muscle soreness. It also helps improve circulation, which can promote healing and reduce stiffness.
You can consume ginger in many forms, including fresh root, powdered spice, tea, or supplements. Fresh ginger can be added to meals, juiced, or boiled into tea, while ginger supplements are available in capsule form. Studies show that a daily dose of 1-2 grams of ginger can effectively reduce pain and inflammation.
However, taking large amounts of ginger may cause mild side effects, like heartburn or stomach discomfort, so moderation is key.
Turmeric
Turmeric is a golden-yellow spice used in folk medicine for centuries. Its active ingredient, curcumin, is a powerful anti-inflammatory and antioxidant compound. Turmeric helps manage chronic pain by targeting pathways involved in inflammation, making it particularly effective for conditions like osteoarthritis, fibromyalgia, and muscle pain.
While turmeric can be used as a spice in cooking, therapeutic benefits often require higher doses, which are achieved through supplements. Curcumin supplements typically provide 500-1000 mg of curcumin per day. To enhance absorption, it’s recommended to consume turmeric with black pepper (containing piperine) or healthy fats.
Turmeric is generally safe, but high doses may cause digestive upset in some individuals. That’s why it’s important to consult a healthcare provider for the correct doses. Adding turmeric tea or supplements to your routine can provide a natural and effective way to manage chronic pain.
Supplements
Supplements can play a vital role in managing chronic pain by addressing nutritional deficiencies and supporting the body’s natural healing processes. Certain supplements, such as omega-3 fatty acids, vitamin D, vitamin B12, and alpha-lipoic acid, have anti-inflammatory and nerve-protecting properties that help reduce pain and promote overall health. When combined with a balanced diet, supplements offer an effective, natural way to manage chronic pain.
Omega-3 Fatty Acids
Omega-3 fatty acids are essential fats that the body cannot produce alone. They are known for their strong anti-inflammatory properties, which help reduce chronic pain caused by arthritis, joint inflammation, and muscle soreness.
Omega-3s decrease the production of inflammatory molecules, such as cytokines and prostaglandins, in the body. They also support overall joint health by improving lubrication and reducing stiffness.
You can naturally obtain omega-3s from fatty fish like salmon, mackerel, and sardines. Plant-based sources include flaxseeds, chia seeds, and walnuts. However, many people opt for fish oil or algae-based supplements for a consistent daily intake. According to the National Institutes of Health, the recommended dose is 1000-1200 mg of EPA and DHA (the active components in omega-3s).
Regular consumption can improve not only pain levels but also cardiovascular and cognitive health.
Vitamin D
Vitamin D is crucial for maintaining strong bones and reducing chronic pain. It helps regulate calcium absorption and supports bone health, alleviating pain associated with osteoporosis, fibromyalgia, and arthritis. Additionally, vitamin D plays a role in modulating the immune system, which helps reduce inflammation that contributes to chronic pain.
Sunlight is the most natural source of vitamin D, with just 10-30 minutes of exposure several times a week being enough for most people. It is also found in foods like fatty fish (salmon, tuna), fortified milk, and egg yolks.
Supplements are often necessary for those with limited sun exposure or a deficiency. According to the National Institutes of Health, the daily dose typically ranges from 600-800 IU, but higher doses may be needed for individuals with severe deficiencies.
Consult a healthcare provider or a functional medicine practitioner for a simple blood test that can determine your vitamin D levels and guide supplementation.
Vitamin B12
Vitamin B12 is essential for nerve health and plays a critical role in managing neuropathic pain. It supports the repair of damaged nerves and improves nerve function, making it particularly useful for conditions like diabetic neuropathy, sciatica, and fibromyalgia. A deficiency in B12 can lead to nerve pain, numbness, and tingling, especially in the hands and feet.
Vitamin B12 is naturally found in animal products like meat, fish, eggs, and dairy, but vegetarians, vegans, and older adults may need supplements to meet their needs. B12 supplements are available in several forms, including tablets, capsules, and sublingual drops. In cases of severe deficiency, injections may be required. According to the National Institutes of Health, the recommended daily dose varies but typically ranges from 1.2-2.4 mcg.
Regular intake can significantly improve nerve health and reduce pain over time.
Alpha Lipoic Acid (ALA)
Alpha-lipoic acid (ALA) is a powerful antioxidant that helps reduce inflammation and nerve pain, especially in conditions like diabetic neuropathy. It works by neutralizing free radicals and improving blood flow to nerves, which can decrease pain and improve nerve function. ALA also enhances the body’s use of insulin, making it beneficial for individuals with diabetes-related pain.
Natural sources of ALA include spinach, broccoli, tomatoes, and red meat, but therapeutic doses often require supplements. According to Dr. Hiep Nguyen from the Christus Health Hospital, Texas, USA, daily dose of 600-1200 mg is commonly recommended for managing chronic pain, particularly nerve pain. ALA is generally well-tolerated, but some individuals may experience mild side effects, such as nausea or dizziness.
Including ALA as part of your supplement routine can provide significant relief for nerve-related chronic pain.
Hot and Cold Therapy
Hot and cold therapy is a simple yet effective way to manage chronic pain by targeting inflammation and improving circulation.
Heat therapy relaxes muscles, increases blood flow, and alleviates stiffness, making it especially useful for chronic conditions like arthritis or back pain. You can use heating pads, warm baths, or heat wraps to deliver soothing warmth to the affected area.
Cold therapy, on the other hand, reduces swelling and numbs sharp pain by constricting blood vessels and calming inflamed tissues. Ice packs, cold compresses, or gel packs are commonly used for acute flare-ups or swelling related to chronic conditions.
Alternating between hot and cold therapy can be particularly beneficial, as it helps reduce pain while promoting healing in the affected tissues.
Yoga and Stretching
Yoga and stretching are powerful tools for managing chronic pain by improving flexibility, posture, and muscle strength. Regular practice helps relieve tension in tight muscles, reduce stiffness, and improve joint mobility. For conditions like fibromyalgia or chronic back pain, gentle yoga poses like cat-cow, child’s pose and targeted stretches can help release pressure on affected areas and enhance overall body function.
Yoga also incorporates controlled breathing and relaxation techniques, calming the nervous system and reducing stress-related pain. Even short daily sessions can improve physical function and reduce pain intensity over time.
Meditation and Mindfulness
Meditation and mindfulness practices help manage chronic pain by addressing its mental and emotional impact. Chronic pain often creates a cycle of stress, anxiety, and heightened sensitivity to discomfort. Mindfulness helps break this cycle by teaching you to focus on the present moment and accept sensations without judgment.
Techniques like body scans, deep breathing, and guided imagery can reduce stress hormones and calm the nervous system, making pain feel less overwhelming. Research shows that mindfulness-based stress reduction (MBSR) programs can lower pain intensity and improve emotional well-being in people with chronic pain conditions.
Regular meditation practice doesn’t just ease pain perception, It also promotes relaxation and a more positive outlook, helping you regain a sense of control over your life.
Frequently Asked Questions
Can Chronic Pain Cause High Blood Pressure?
Yes, chronic pain can cause high blood pressure (hypertension). Persistent pain activates the body’s stress response, releasing hormones like adrenaline and cortisol that increase heart rate and constrict blood vessels. Over time, this sustained stress can lead to elevated blood pressure. Managing chronic pain effectively may help reduce its impact on your cardiovascular health.
Does Chronic Pain Cause Depression?
Yes, chronic pain is closely linked to depression. Research by Dr. Jiyao Sheng from the Second Hospital of Jilin University, China shows that “Pain and depression are closely correlated from the perspectives of both brain regions and the neurological function system.”
The constant discomfort and limitations on daily activities can lead to feelings of hopelessness, frustration, and sadness. Additionally, the same brain chemicals that regulate mood are also involved in pain processing, creating a two-way relationship between chronic pain and depression. Treating both conditions together often provides better results.
What Is The Difference Between Acute And Chronic Pain?
The difference between acute and chronic pain is that acute pain is short-term and usually linked to an injury or illness, signaling the body to take action to heal. It resolves once the underlying issue is treated. Chronic pain lasts over three months and may persist even after the initial cause is resolved. Unlike acute pain, chronic pain often involves changes in the nervous system, making it harder to manage.
Does Chronic Pain Cause Fatigue?
Yes, chronic pain frequently causes fatigue. The body uses extra energy to cope with persistent discomfort, and pain often disrupts sleep, preventing adequate rest. This combination leads to physical and mental exhaustion, making it difficult to carry out daily tasks or maintain a healthy lifestyle. Addressing both pain and sleep issues such as sleep apnea and insomnia is key to reducing fatigue.
Can Anxiety Cause Chronic Pain?
Yes, anxiety can contribute to chronic pain. High anxiety levels can lead to muscle tension, increased pain sensitivity, and a heightened stress response, all of which can amplify existing pain or even create new pain symptoms. Conditions like tension headaches, back pain, or fibromyalgia are often linked to anxiety. Managing anxiety through therapy, relaxation techniques, or mindfulness can help alleviate chronic pain.
Conclusion
Living with chronic pain is a daily struggle- sleepless nights, limited mobility, and the emotional toll of constant discomfort can make even simple tasks feel overwhelming.
But chronic pain doesn’t have to define your life.
Natural treatments, such as functional medicine, dietary adjustments, herbal remedies, and supplements, effectively manage pain and restore balance. Therapies like hot and cold treatments, yoga, and mindfulness can further enhance relief by reducing inflammation, improving mobility, and calming your mind.
Understanding the root causes of your pain is the first step to long-lasting solutions.
At the Bay Clinic of Chiropractic in Panama City, Florida, Dr. Tony Salamay is committed to helping you break free from the cycle of chronic pain. As a skilled chiropractor, nutritionist, and functional medicine expert, Dr. Salamay offers personalized care tailored to your unique challenges. He focuses on addressing the root causes of pain, whether it’s inflammation, misalignment, or lifestyle factors, to help you regain control and live with vitality.
Don’t let chronic pain hold you back any longer. Contact the Bay Clinic of Chiropractic at (850) 785-9372 or info@thebaydoctor.com today!
Your healing journey begins here with care designed just for you.
References
- Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-Based survey. Journal of Pain [Internet]. 2010 Aug 27;11(11):1230–9. Available from: https://www.jpain.org/article/S1526-5900%2810%2900601-2/fulltext
- Stretanski MF, Kopitnik NL, Matha A, Conermann T. Chronic pain [Internet]. StatPearls – NCBI Bookshelf. 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553030/
- Rodríguez I, Abarca E, Herskovic V, Campos M. Living with Chronic Pain: A Qualitative Study of the Daily Life of Older People with Chronic Pain in Chile. Pain Research and Management [Internet]. 2019 Apr 1;2019:1–9. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6466839/
- Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, et al. Neuropathic pain. Nature Reviews Disease Primers [Internet]. 2017 Feb 15;3(1):17002. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5371025/
- Dydyk AM, Chiebuka E, Stretanski MF, Givler A. Central Pain Syndrome [Internet]. StatPearls – NCBI Bookshelf. 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553027/
- Westlund KN. Visceral nociception. Current Review of Pain [Internet]. 2000 Dec 1;4(6):478–87. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7879461/
- Schneider S, Junghaenel DU, Keefe FJ, Schwartz JE, Stone AA, Broderick JE. Individual differences in the day-to-day variability of pain, fatigue, and well-being in patients with rheumatic disease: Associations with psychological variables. Pain [Internet]. 2012 Feb 19;153(4):813–22. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3307888/
- Maldonado RJ, De Jesus O. Hyperesthesia [Internet]. StatPearls – NCBI Bookshelf. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563125/
- Eccles JA, Davies KA. The challenges of chronic pain and fatigue. Clinical Medicine [Internet]. 2021 Jan 1;21(1):19–27. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7850224/
- Hu J, Bortsov AV, Ballina L, Orrey DC, Swor RA, Peak D, et al. Chronic widespread pain after motor vehicle collision typically occurs through immediate development and nonrecovery. Pain [Internet]. 2015 Oct 22;157(2):438–44. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4942849/
- Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, et al. Diabetic neuropathy. Nature Reviews Disease Primers [Internet]. 2019 Jun 13;5(1):42. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7096070/
- Cohen SP, Wang EJ, Doshi TL, Vase L, Cawcutt KA, Tontisirin N. Chronic pain and infection: mechanisms, causes, conditions, treatments, and controversies. BMJ Medicine [Internet]. 2022 Mar 1;1(1):e000108. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10012866/
- Elma Ö, Brain K, Dong HJ. The importance of nutrition as a lifestyle factor in chronic Pain Management: A Narrative review. Journal of Clinical Medicine [Internet]. 2022 Oct 9;11(19):5950. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9571356/
- Pahwa R, Goyal A, Jialal I. Chronic inflammation [Internet]. StatPearls – NCBI Bookshelf. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493173/
- Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organization Journal [Internet]. 2012 Jan 1;5(1):9–19. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3488923/
- Krupa KN, Fritz K, Parmar M. Omega-3 fatty acids [Internet]. StatPearls – NCBI Bookshelf. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564314/
- Asensi MT, Napoletano A, Sofi F, Dinu M. Low-Grade Inflammation and Ultra-Processed Foods Consumption: A review. Nutrients [Internet]. 2023 Mar 22;15(6):1546. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10058108/
- Sarkar D, Jung MK, Wang HJ. Alcohol and the immune system [Internet]. 2015. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4590612/
- Senzon SA. The Chiropractic Vertebral Subluxation Part 1: Introduction. Journal of Chiropractic Humanities [Internet]. 2018 Dec 1;25:10–21. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6472118/
- Leung KY, Chu ECP, Yau KHY, Ing SNG, Bellin D. RESOLUTION OF CERVICAL RADICULOPATHIC SYMPTOMS AND RESTORATION OF NORMAL CERVICAL LORDOSIS IN a 20 YEAR OLD FEMALE: a CASE REPORT [Internet]. Published in Journal of Contemporary Chiropractic. 2022. Available from: https://journal.parker.edu/article/78051-resolution-of-cervical-radiculopathic-symptoms-and-restoration-of-normal-cervical-lordosis-in-a-20-year-old-female-a-case-report
- Chaibi A, Stavem K, Russell MB. Spinal Manipulative Therapy for Acute Neck Pain: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Journal of Clinical Medicine [Internet]. 2021 Oct 28;10(21):5011. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8584283/
- Lin CR, Tsai SHL, Wang C, Lee CL, Hung SW, Ting YT, et al. Willow Bark (Salix spp.) Used for Pain Relief in Arthritis: A Meta-Analysis of Randomized Controlled Trials. Life [Internet]. 2023 Oct 14;13(10):2058. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10607963/
- Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arteriosclerosis Thrombosis and Vascular Biology [Internet]. 2011 Apr 20;31(5):986–1000. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3081099/
- Bischoff-Kont I, Fürst R. Benefits of ginger and its constituent 6-Shogaol in inhibiting inflammatory processes. Pharmaceuticals [Internet]. 2021 Jun 15;14(6):571. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8232759/
- Black CD, Herring MP, Hurley DJ, O’Connor PJ. Ginger (Zingiber officinale) Reduces Muscle Pain Caused by Eccentric Exercise. Journal of Pain [Internet]. 2010 Apr 26;11(9):894–903. Available from: https://www.jpain.org/article/S1526-5900%2809%2900915-8/fulltext?
- Paultre K, Cade W, Hernandez D, Reynolds J, Greif D, Best TM. Therapeutic effects of turmeric or curcumin extract on pain and function for individuals with knee osteoarthritis: a systematic review. BMJ Open Sport & Exercise Medicine [Internet]. 2021 Jan 1;7(1):e000935. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7812094/
- Boonrueng P, Wasana PWD, Hasriadi N, Vajragupta O, Rojsitthisak P, Towiwat P. Combination of curcumin and piperine synergistically improves pain-like behaviors in mouse models of pain with no potential CNS side effects. Chinese Medicine [Internet]. 2022 Oct 23;17(1). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9590184/
- Calder PC. Omega-3 fatty acids and inflammatory processes. Nutrients [Internet]. 2010 Mar 18;2(3):355–74. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3257651/
- Office of Dietary Supplements – Omega-3 fatty acids [Internet]. Available from: https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/
- Mohebi-Nejad A, Bikdeli B. Omega-3 supplements and cardiovascular diseases [Internet]. 2014. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4153275/
- Kragstrup TW. Vitamin D supplementation for patients with chronic pain. Scandinavian Journal of Primary Health Care [Internet]. 2010 Nov 15;29(1):4–5. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3347929/
- Office of Dietary Supplements – Vitamin D [Internet]. Available from: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Julian T, Syeed R, Glascow N, Angelopoulou E, Zis P. B12 as a treatment for Peripheral Neuropathic pain: A Systematic review. Nutrients [Internet]. 2020 Jul 25;12(8):2221. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7468922/
- Office of Dietary Supplements – Vitamin B12 [Internet]. Available from: https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- Viana MDM, Lauria PSS, De Lima AA, Opretzka LCF, Marcelino HR, Villarreal CF. Alpha-Lipoic acid as an antioxidant strategy for managing neuropathic pain. Antioxidants [Internet]. 2022 Dec 8;11(12):2420. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9774895/
- Nguyen H, Pellegrini MV, Gupta V. Alpha-Lipoic acid [Internet]. StatPearls – NCBI Bookshelf. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564301/
- French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. Superficial heat or cold for low back pain. Cochrane Database of Systematic Reviews [Internet]. 2006 Jan 20;2011(2):CD004750. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8846312/
- Chopra D, Stern E, Bushell WC, Castle RD. Yoga and pain: A mind-body complex system. Frontiers in Pain Research [Internet]. 2023 Feb 23;4:1075866. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9996306/
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness Meditation for Chronic Pain: Systematic review and Meta-analysis. Annals of Behavioral Medicine [Internet]. 2016 Sep 22;51(2):199–213. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5368208/
- Sheng J, Liu S, Wang Y, Cui R, Zhang X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plasticity [Internet]. 2017 Jan 1;2017:1–10. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5494581/